Does precision really matter?
Before we discuss about accuracy of CAIS however, we will need to note that the actual guided surgery is only one final step of a long sequence in a digital workflow. This workflow includes a lot of steps, each of them with potential for errors.
- First, we rely on a CBCT. Unlike what you might think, the 3D image of the CBCT software we work with in our computer screens is not a radiographic image. It is an algorithmic reconstruction of many radiographic images. Every algorithm will use certain calculated “approximations” and might not always be absolutely loyal to the true anatomy. Importing the DICOM file to the treatment planning software invites one more algorithm in the party.
- Then transposing the STL file from the optical scan and the essential rendering has the potential to further influence dimensions. Finally, 3D printing of a surgical guide is a workflow step with potential to introduce some more distortion. Conclusively, by the time we are about to use our CAIS system to place the implant, there is already some accumulated error from the workflow, that even if the CAIS was to be perfect, we would still observe some deviation from the planned position.
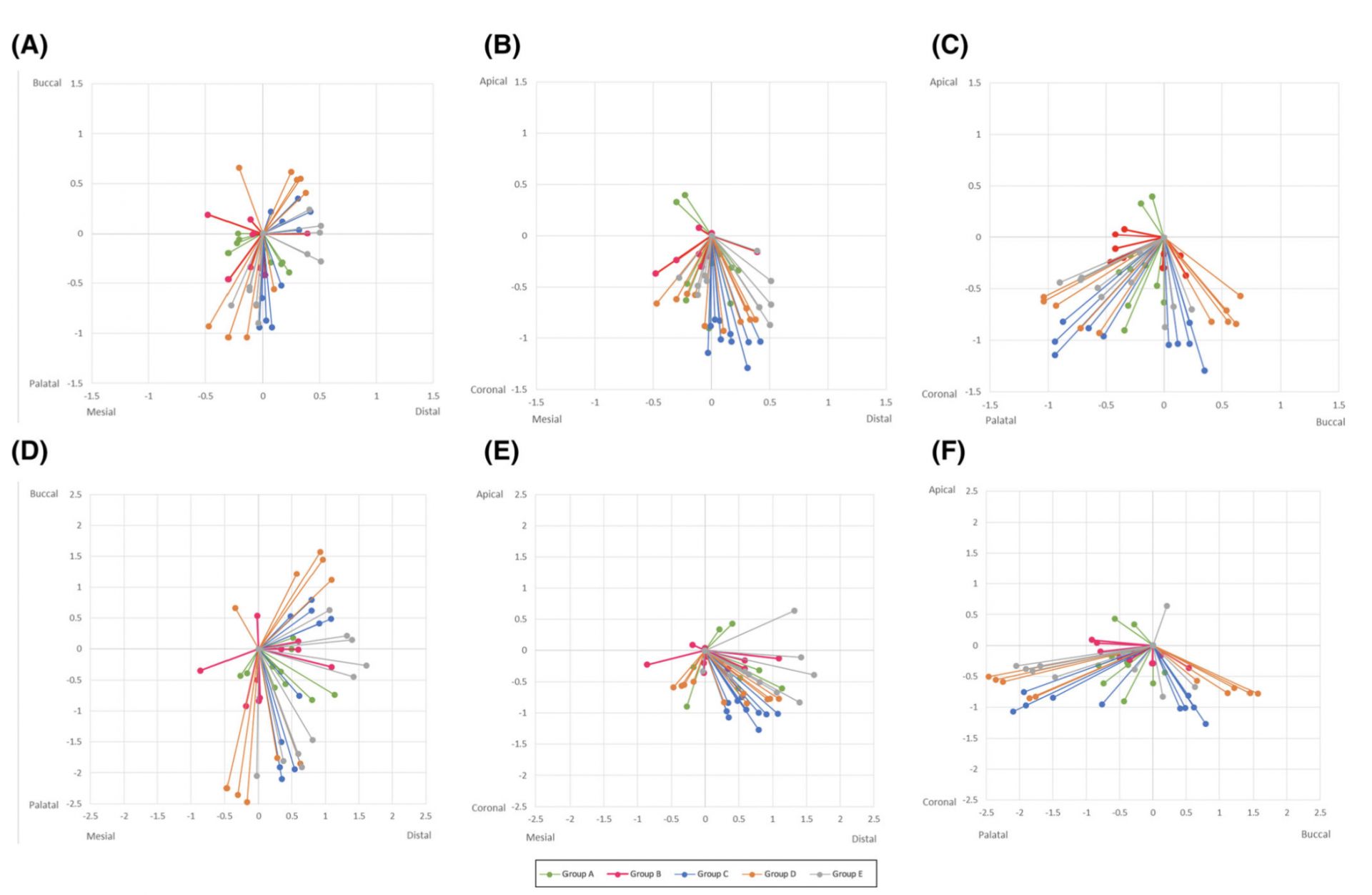
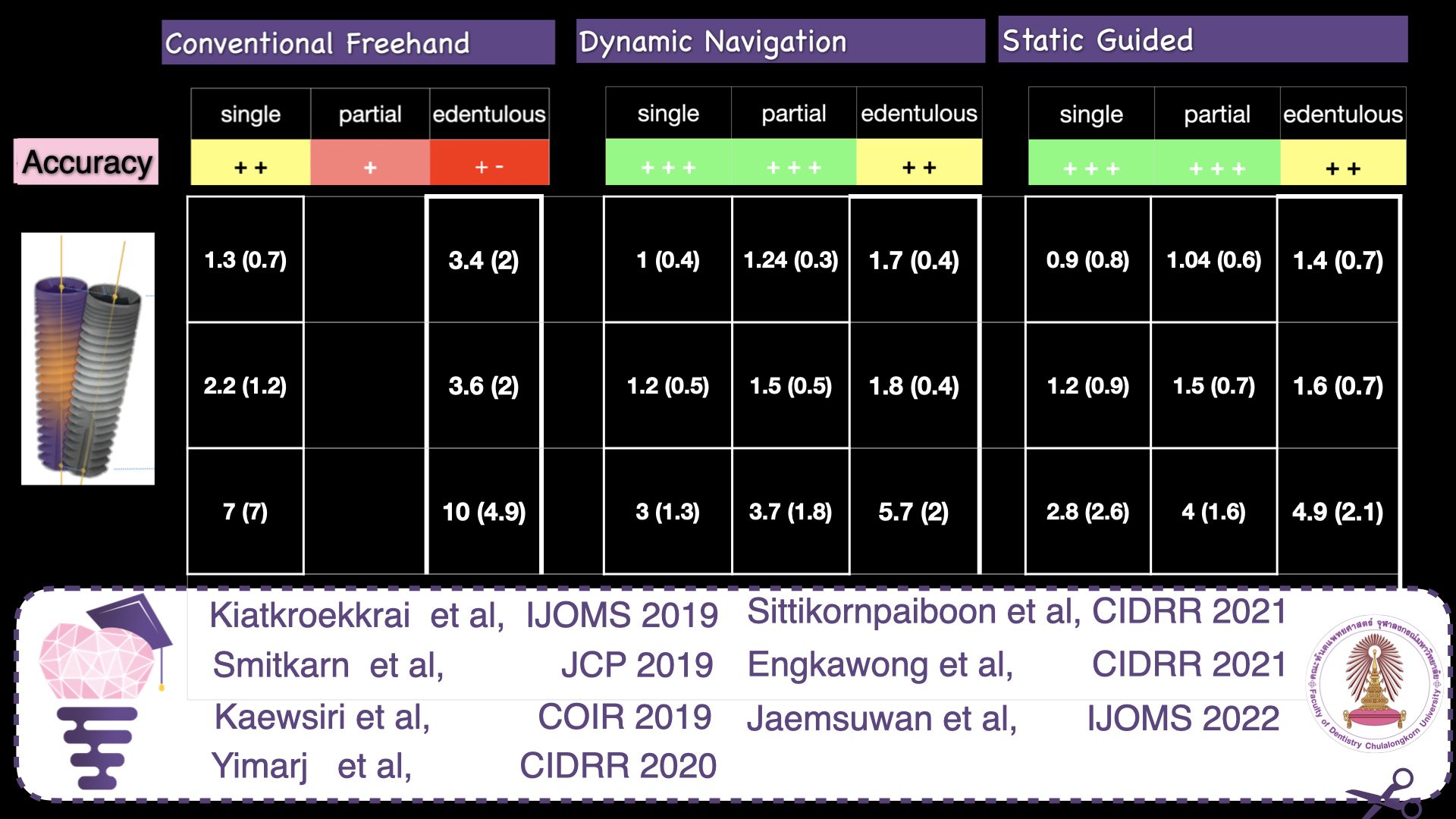
Back to the main point now: how accurate is implant placement when we use CAIS?To answer this we can see the results accumulated through a major CAIS research project in the OMFS clinic at Chulalongkorn University in the past 3 years. This project has by now involved more than 200 patients and included research protocols in many different clinical scenaria. The strength of this project is that by standardizing the studies and using the same technology and software, the same operators , clinic set up, as well as the same patient pool , we can at least ensure that the workflow error is similar in all cases thus the observed differences can be attributed to the clinical conditions we investigate. Compiled from a series of same-workflow RCTs, this table from Chulalongkorn University now shows a clear trend with the accuracy of CAIS being closer to this of conventional freehand placement at single gaps, while the deviation drastically increases as we move to partially and fully edentulous patients. The deviation also trends to be slightly higher in dynamic than static guided when we are dealing with partially and fully edentulous cases, but at the same time both static and dynamic CAIS perform increasingly (and significantly) better than freehand placement, as complexity increases. Of course, accuracy is just the tip of the iceberg and decision making involves several other clinical outcomes, cost effectiveness, many aspects of efficiency, surgical anatomy and site characteristics, learning curve, patient reported outcomes and more...
- First, we rely on a CBCT. Unlike what you might think, the 3D image of the CBCT software we work with in our computer screens is not a radiographic image. It is an algorithmic reconstruction of many radiographic images. Every algorithm will use certain calculated “approximations” and might not always be absolutely loyal to the true anatomy. Importing the DICOM file to the treatment planning software invites one more algorithm in the party.
- Then transposing the STL file from the optical scan and the essential rendering has the potential to further influence dimensions. Finally, 3D printing of a surgical guide is a workflow step with potential to introduce some more distortion. Conclusively, by the time we are about to use our CAIS system to place the implant, there is already some accumulated error from the workflow, that even if the CAIS was to be perfect, we would still observe some deviation from the planned position.
Back to the main point now: how accurate is implant placement when we use CAIS?To answer this we can see the results accumulated through a major CAIS research project in the OMFS clinic at Chulalongkorn University in the past 3 years. This project has by now involved more than 200 patients and included research protocols in many different clinical scenaria. The strength of this project is that by standardizing the studies and using the same technology and software, the same operators , clinic set up, as well as the same patient pool , we can at least ensure that the workflow error is similar in all cases thus the observed differences can be attributed to the clinical conditions we investigate. Compiled from a series of same-workflow RCTs, this table from Chulalongkorn University now shows a clear trend with the accuracy of CAIS being closer to this of conventional freehand placement at single gaps, while the deviation drastically increases as we move to partially and fully edentulous patients. The deviation also trends to be slightly higher in dynamic than static guided when we are dealing with partially and fully edentulous cases, but at the same time both static and dynamic CAIS perform increasingly (and significantly) better than freehand placement, as complexity increases. Of course, accuracy is just the tip of the iceberg and decision making involves several other clinical outcomes, cost effectiveness, many aspects of efficiency, surgical anatomy and site characteristics, learning curve, patient reported outcomes and more...
Is system precision different to accuracy and why should we care?